Consider the medical necessity form not merely as paperwork, but as the essential protocol that unlocks your premier global health benefits. For discerning expatriates and high-net-worth individuals, this document is the critical communication channel between your physician and your insurer.
It provides the formal, evidence-based rationale for why a specific treatment, an advanced procedure, or a specialty medication is not just advisable, but imperative for your health.
Why the Medical Necessity Form Is Crucial for Global Professionals

As a globally mobile professional, your healthcare requirements transcend international borders. While you expect seamless access to world-class care, insurance providers operate on a foundation of rigorous validation. This is precisely where the medical necessity form becomes indispensable.
This form translates your physician's clinical judgment into the precise language your insurer understands and accepts. It is the formal justification for their recommended course of action. Without this documented proof, even the most essential procedures can be stalled in approval processes or face an outright denial.
Safeguarding Your Health and Financial Portfolio
Mastering this process is more than an administrative task; it is a strategic imperative. A properly executed medical necessity form ensures your care is approved without friction, protecting both your well-being and your financial portfolio from unexpected and significant liabilities. This is particularly true when engaging with high-cost treatments or consultations with specialists outside your primary network.
This requirement is becoming more critical as global medical costs continue their upward trajectory. The 2025 Global Medical Trends Survey projects a global average medical trend rate of 9.3% in 2025. In response, insurers are naturally intensifying their review protocols. This trend means that clear, detailed medical necessity documentation is no longer optional—it is essential to substantiate coverage.
A well-prepared medical necessity form is more than a request. It is a strategic instrument for ensuring your care is approved without delay, aligning your medical needs with your policy's framework.
By understanding its role, you can assume command of your healthcare journey. It is a key step in realising the full value of your benefits, a subject we explore further in our guide to international private medical insurance benefits. This knowledge empowers you to proceed with confidence, no matter where your professional life leads.
Knowing When a Medical Necessity Form Is Required
Anticipating when your insurer will request a medical necessity form is fundamental to managing your healthcare proactively. This foresight prevents frustrating delays in care and unwelcome claim denials, ensuring your health journey proceeds smoothly.
Consider it akin to planning a complex itinerary; understanding the critical checkpoints in your insurance process is paramount.
In my experience, this form is typically required in three specific scenarios, each designed to validate the necessity of your care.
Securing Pre-Authorisation for Planned Procedures
For any significant, non-emergency procedure, pre-authorisation is a standard requirement. This is the insurer's method of confirming that a planned treatment—such as specialised cardiac surgery in another country or an advanced orthopaedic operation—is medically justified before they commit to covering the cost.
The medical necessity form is the cornerstone of this process. It presents your physician's detailed argument for the treatment's necessity, allowing the insurer to approve the expense upfront. Neglecting this step can be a costly oversight, potentially leaving you liable for substantial out-of-pocket expenses for a procedure the insurer deems unjustified.
Justifying Claims After Emergency Care
In a genuine medical emergency, time does not permit pre-authorisation. However, the need for justification is not eliminated—it is merely deferred. Following stabilisation and urgent care, the insurer will require a retrospective review to process the claim.
This is where the medical necessity form provides clarity. It articulates precisely why the emergency services were vital, linking your diagnosis to the treatment administered. Without this formal report, insurers may question the extent of care provided, leading to claim disputes.
Obtaining Approval for Out-of-Network Specialists
It is common for discerning individuals to seek the expertise of leading physicians or world-renowned clinics that are not within their plan's established network. However, insurers will not cover out-of-network care without a compelling reason.
A medical necessity form serves as your physician's formal case, explaining why a particular out-of-network specialist is uniquely qualified and indispensable for your condition. This documentation is especially critical when navigating complex policy exclusions and conditions that might otherwise restrict your options.
The importance of these forms has grown with the increasing complexity of healthcare, particularly with the advent of high-cost specialty pharmaceuticals. Globally, innovative medicines for conditions like cancer are a significant driver of medical expenses. Consequently, insurers increasingly rely on rigorous medical necessity reviews to manage pharmacy costs, demanding precise evidence before approving coverage for such treatments.
The Anatomy of a Flawless Medical Necessity Form
View a medical necessity form not as a bureaucratic impediment, but as a meticulously constructed case presented to your insurer. An exemplary submission is clear, compelling, and leaves no room for ambiguity. Perfecting it the first time is essential to avoid frustrating delays and denials.
This is the medium through which your physician translates their professional judgment into the language of insurance. It requires more than completing fields; it involves building an unassailable case for the care you require. Every detail, from standardised codes to the clinical narrative, must be precise.
The Core Informational Pillars
A robust form is built upon several key pillars of information. An error in one can compromise the entire structure. In my experience, incomplete or vague information is the leading cause of initial rejections, initiating a cycle of appeals and lost time.
The form must begin with specific, universally recognised codes that provide a concise summary of your condition and the proposed treatment.
- Diagnostic Codes (ICD-10): This defines the "what." The form requires the precise International Classification of Diseases, 10th Revision (ICD-10) code that identifies your medical condition. A generic diagnosis such as "back pain" is insufficient; the code must reflect the specific pathology driving the need for care.
- Procedural Codes (CPT): This defines the "how." The Current Procedural Terminology (CPT) code details the exact medical service, procedure, or test being recommended. Accuracy is critical, as it directly corresponds to the insurer's payment schedules and coverage guidelines.
Building the Clinical Narrative
Codes are only the foundation. The substance of the form lies in the clinical rationale that connects your diagnosis to the recommended treatment. This is your physician's opportunity to advocate on your behalf, explaining why a specific intervention is not merely an option, but medically essential.
This justification must include a summary of your patient history, a record of previous treatments and their outcomes, and a clear argument for why the proposed treatment is the logical and necessary next step. The strength of this narrative is often the deciding factor between a swift approval and a denial.
This entire process is grounded in the principles of evidence-based medicine. Insurers utilize health statistics that track risks and outcomes across large populations to develop their policies. This data-driven approach ensures that a requested service aligns with established clinical guidelines, ultimately protecting you from ineffective or unnecessary treatments.
To assist you and your physician in constructing an irrefutable case, I have outlined the essential components of the form in the table below. Consider it a checklist to ensure every element of your submission is impeccable.
Key Components of a Medical Necessity Form
This table details the crucial elements of the form, explaining the strategic purpose of each and providing a best-practice example.
| Component | Purpose | Example of Information Required |
|---|---|---|
| Patient Demographics | Ensures accurate identification and links the form to the correct insurance policy. | `Full Name: Jane A. Doe |
| Diagnostic Code (ICD-10) | Provides a universal, specific classification of the medical condition being treated. | M54.5 (Low back pain) |
| Procedural Code (CPT) | Specifies the exact medical service or procedure requested for reimbursement. | 97140 (Manual therapy techniques, 1 or more regions, each 15 minutes) |
| Physician's Rationale | Delivers the clinical justification explaining why the treatment is necessary now. | "Patient has failed 8 weeks of conservative treatments... See notes below." |
| Treatment History | Documents previous interventions to prove the proposed treatment is a logical next step. | "6 weeks of physical therapy yielded minimal improvement in pain scores." |
| Supporting Documents | Provides objective evidence like imaging, lab results, or specialist reports. | MRI report dated 10/25/2024 showing L4-L5 disc herniation. |
Correctly addressing these components transforms the form from a simple request into a powerful, evidence-backed argument for your care. It is the difference between asking for approval and demonstrating why it is the only logical outcome.
A Strategic Approach to the Submission Process
Approach the submission of a medical necessity form not as a task, but as the management of a high-stakes project. This shift in mindset is crucial for success. This approach elevates you from a passive patient to the active director of your healthcare approval, ensuring every detail is perfectly aligned for a first-pass approval.
Your primary point of contact is your physician's office. However, it is a critical error to assume they understand the specific nuances of your international health plan. It is your responsibility to provide this context. Doing so empowers them to construct a more robust and targeted justification on your behalf.
Proactively Managing the Submission
Clear, precise communication is paramount. A concise email or brief call to your physician's administrative team can be highly effective. Simply outline the key points your insurer requires. This simple act of alignment can prevent the common errors that lead to immediate rejections.
For example, a vague clinical narrative is a classic reason for failure. Instead of allowing a general statement, guide your physician’s office to articulate why a specific treatment is necessary for your unique situation. They must also explain why standard in-network options are clinically inappropriate. This level of detail is not optional; it is essential.
The entire process depends on three key elements working in harmony: your patient information, the correct medical codes, and a compelling clinical narrative.
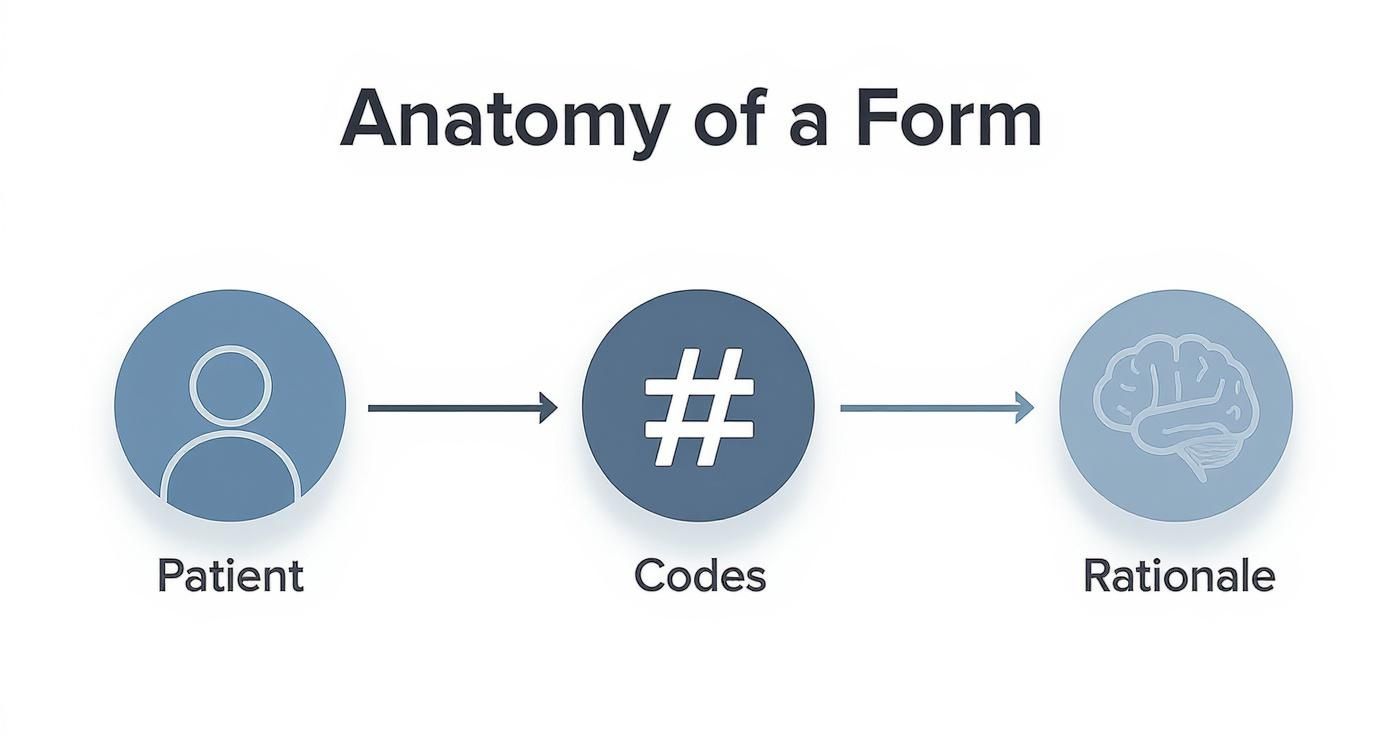
As the diagram illustrates, these three components must interlock perfectly to create a persuasive justification that is resistant to insurer scrutiny.
Avoiding Common Submission Pitfalls
Several predictable mistakes can derail an otherwise solid medical necessity claim. By anticipating them, you can ensure your submission is flawless from the outset.
- Incomplete Medical Records: Ensure every supporting document—such as recent lab results, specialist notes, or imaging reports—is included. Without evidence, your justification is merely an opinion.
- Coding Discrepancies: A mismatch between the diagnosis code (ICD-10) and the procedure code (CPT) is a significant red flag for insurance reviewers. Always verify that the proposed treatment is a direct and logical consequence of the diagnosis.
- Ignoring Pre-Authorisation Timelines: Submitting a form after the specified deadline results in an automatic denial. You can learn more about managing these timelines in our deep dive into pre-authorisation and direct settlement.
A successful submission is one that anticipates and addresses every potential question the insurer might have. This level of preparation leaves no room for doubt and builds an undeniable, evidence-backed case for approval.
Furthermore, these forms contain highly sensitive information. It is prudent to understand the features of robust healthcare data security solutions to ensure your personal health data is protected throughout this process.
By adopting this project manager mindset, you take firm control, steering the entire process toward a swift and positive outcome.
How Your Broker Can Expedite Critical Approvals

For busy professionals managing global health, a specialized insurance broker is not merely an administrator—they are an indispensable advocate. Their value is most apparent when navigating the approval process for a medical necessity form, transforming a potentially arduous ordeal into a streamlined success.
Think of an experienced broker as your personal liaison with the insurance carrier. They are a dedicated partner who understands the intricate criteria of internal review boards and, equally important, the unwritten rules that often influence approval decisions.
This institutional knowledge is a formidable advantage. While you see a generic submission portal, your broker sees a network of professional relationships cultivated over many years.
Leveraging Relationships for Rapid Resolution
When a medical necessity form encounters a delay or query, the standard process can grind to a halt. An individual could spend weeks caught in a loop of automated phone systems and vague email responses.
In contrast, an expert broker can often navigate such complexities in a fraction of the time. They do not wait in the general queue. They leverage established contacts to connect directly with the case managers or underwriting decision-makers who can resolve the issue.
This direct line of communication is essential for clarifying complex clinical details or providing supplementary information without the significant delays inherent in the standard process.
A proactive broker does not just manage paperwork; they actively champion your case. They anticipate the insurer's questions, assist in framing the clinical narrative for maximum impact, and know precisely whom to contact to escalate the issue for a swift, favorable outcome.
This level of hands-on intervention is particularly vital when dealing with high-stakes procedures in foreign countries, where differences in medical terminology or documentation standards can easily create friction.
An Example of Broker Intervention in Action
Consider an expatriate in Singapore scheduled for a specialized spinal procedure. Her surgeon submits the medical necessity form, but the insurer's U.S.-based review team flags it, citing unfamiliarity with the specific surgical technique described.
Facing this alone, the expatriate would be mired in a frustrating exchange, attempting to bridge the communication gap between two different healthcare systems.
A skilled broker, however, intervenes immediately. They contact their dedicated representative at the insurance company, facilitate a direct peer-to-peer call between the Singaporean surgeon and the insurer’s medical director, and ensure the clinical evidence is presented in a manner the review board understands and accepts.
What could have been a multi-week stalemate is resolved in under 48 hours. The procedure is approved, and the patient’s care proceeds without delay. This is the tangible value of having a dedicated advocate.
Common Questions About the Medical Necessity Process
Even with meticulous preparation, the medical necessity process can present challenges. Here are answers to some of the most common questions, providing direct, actionable information to keep your healthcare on track.
How Long Does Approval Typically Take?
The timeline for approval varies based on the insurer and the complexity of the request.
For a straightforward pre-authorisation with a complete and accurate submission, approval can often be secured within 3-5 business days.
However, for more complex cases—such as those involving an out-of-network specialist or a novel treatment—the review process can extend to 10-15 business days, or longer. The most critical factor for an expedited turnaround is the quality of the initial submission. Any request for additional information effectively resets the review clock.
What Is the Appeals Process for a Denied Form?
First, a denial should not be viewed as a final decision, but rather as the beginning of the next phase.
Your first step is to obtain the denial in writing from the insurer, which must specify the exact reason for the decision. Common reasons include missing documentation, a coding error, or a clinical determination that the treatment was not necessary based on the evidence provided.
With this information, you and your physician can construct a more robust case for appeal. This may involve providing additional clinical evidence, referencing relevant medical studies, or rewriting the original justification for greater clarity. This is a scenario where an experienced broker is invaluable; they understand how to frame the appeal and ensure it reaches the appropriate reviewers.
A denial is not a final verdict. It is an opportunity to present a more compelling argument. A well-constructed appeal has a significant probability of overturning the initial decision.
Can I Use One Form for Care in Different Countries?
No, a medical necessity form is specific to a single treatment from a particular physician or facility. If your healthcare journey involves multiple providers across different countries, each step requires a separate submission.
For instance:
- A consultation with a specialist in Switzerland requires one form.
- A subsequent procedure with a surgeon in Germany requires a new, distinct form.
Each provider must justify their recommended treatment based on their own clinical assessment. For individuals coordinating global care, managing these submissions sequentially is critical to ensuring continuous, uninterrupted coverage.
At Riviera Expat, we specialise in the complexities of international health insurance. We provide the expert guidance and dedicated advocacy required to navigate the administrative landscape. Our objective is to ensure you receive the best possible care, without the associated administrative burdens. Contact us today for a complimentary consultation to ensure your global health strategy is as sophisticated as your professional one.

