A medical deductible is the portion of your healthcare expenses you agree to cover personally before your insurance carrier begins to contribute. It is not a fee or a penalty; it is the cornerstone of the cost-sharing agreement you establish with your insurer.
What Is a Medical Deductible?
For individuals accustomed to managing a financial portfolio, a medical deductible is a strategic lever for controlling costs and managing personal risk exposure. When selecting a deductible, you set a specific monetary threshold. You are responsible for all medical costs up to that amount; only then does your insurer's coverage activate for more substantial expenses.
This is a fundamental principle in both domestic plans and International Private Medical Insurance (IPMI). It establishes a clear demarcation: you cover the initial, more predictable costs, while your insurer provides a safeguard against larger, less foreseeable medical events.
The Financial Mechanics of a Deductible
The relationship between your deductible and your monthly insurance payment—the premium—is an explicit trade-off.
If you opt for a higher deductible, you signal to the insurer a willingness to assume a greater share of the initial financial risk. They, in turn, reward this with a lower monthly premium. It is a direct and logical exchange.
Conversely, a lower deductible means the insurer is liable for costs much sooner. To compensate for this elevated risk, they will charge a higher premium. We delve deeper into the nuanced distinctions between excesses and deductibles in our detailed guide.
This trade-off is central to structuring your coverage. If you are in excellent health and anticipate infrequent medical consultations, a high-deductible plan can yield significant premium savings. However, if you are managing a chronic condition, a lower deductible may be more prudent, providing quicker access to your full benefits.
To illustrate this with precision, consider how a different deductible choice directly impacts your outlay. Note how a higher deductible corresponds to a markedly lower annual premium.
Deductible Impact on Annual Health Insurance Costs
| Plan Tier | Annual Deductible | Monthly Premium | Total Annual Premium |
|---|---|---|---|
| Low Deductible Plan | $500 | $450 | $5,400 |
| Mid Deductible Plan | $2,500 | $300 | $3,600 |
| High Deductible Plan | $5,000 | $225 | $2,700 |
As demonstrated, accepting a higher initial out-of-pocket risk can reduce your fixed insurance costs by as much as 50%. This is a powerful tool for aligning your coverage with your financial strategy and health profile.
A Growing Trend in Cost-Sharing
As global healthcare costs continue their upward trajectory, insurers and employers are increasingly leveraging higher deductibles to maintain manageable premiums. This is not a niche tactic but an emerging standard.
In the United States, for example, the average deductible for single coverage in employer-sponsored plans reached $1,735 in 2023, according to the Kaiser Family Foundation's annual survey. More revealingly, 31% of covered workers in these plans now face an individual deductible of $2,000 or more. The message is unequivocal: policyholders are expected to assume a greater portion of initial healthcare costs.
In essence, your deductible serves as the gatekeeper to your full insurance benefits. It is the predetermined amount you pay out-of-pocket, giving you direct control over the balance between your immediate premium costs and your potential future medical expenses.
How Your Deductible Works in Practice
Understanding the definition of a deductible is foundational. Observing its practical application is what truly impacts your financial position.
In practice, deductibles vary in their structure. The specific design of your plan—when and how often you are required to pay—is the primary determinant of your out-of-pocket costs. The two most common variants, particularly in international plans, are the annual deductible and the per-claim deductible. While they sound similar, their effect on your cash flow throughout the year is profoundly different.
Annual Deductible: The Yearly Hurdle
The annual deductible is the most straightforward and prevalent model. It can be conceptualised as a single financial threshold to be met each policy year.
You pay for all covered medical care out-of-pocket until the cumulative amount you have spent reaches your deductible. Once this threshold is met, your insurer begins to pay its share for the remainder of that policy year.
Let us examine a practical example:
- Your Plan: You hold a policy with a $5,000 annual deductible.
- January Bill: A minor procedure costs $2,000. You pay the full $2,000. You have now satisfied $2,000 of your $5,000 deductible.
- June Bill: You require diagnostic scans costing $3,500. You pay the first $3,000 of this bill. This brings your annual total to $5,000 ($2,000 + $3,000). Your deductible is now met.
- Subsequent Actions: For the remainder of that policy year, your insurer assumes financial responsibility. They will cover the final $500 from the June bill and any other approved medical costs, in accordance with your plan's terms.
This structure provides a high degree of predictability. Once the annual hurdle is cleared, you are substantially protected against any further significant medical bills during that year.
Per-Claim Deductible: The Event-Based Model
A per-claim deductible, sometimes referred to as a per-event deductible, operates on a completely different basis. Instead of a single annual total, you are subject to a separate deductible for each distinct medical condition or incident.
This can be a strategic choice if your primary concern is a single, complex condition that may require extensive treatment. However, if you experience several unrelated health issues within a year, you may find yourself paying the deductible multiple times.
Consider the following scenario:
- Your Plan: You have a policy with a $1,000 per-claim deductible.
- March Incident: You sustain a wrist fracture, with treatment totaling $4,000. You pay the $1,000 deductible for this claim, and the insurer covers the remaining $3,000.
- August Incident: You develop an unrelated dermatological condition requiring tests and a consultation, costing $1,800. As this is a new and distinct claim, you must pay the $1,000 deductible again. The insurer then covers the final $800.
With this model, your total out-of-pocket expenditure can accumulate significantly if you have multiple, unrelated medical needs in one year.
It is absolutely critical to understand what occurs after you meet your deductible. It does not signify that your healthcare becomes free of charge. It simply means you have unlocked the insurer's cost-sharing contributions.
Once your deductible is satisfied, you enter the cost-sharing phase of your plan. This is where terms like coinsurance (you pay a percentage, e.g., 20%, and the insurer pays 80%) or copayments (a fixed fee for a specific service) become relevant. These smaller payments continue until you reach your plan's annual out-of-pocket maximum—the absolute ceiling on what you will spend on covered medical care in a year.
The Strategic Link Between Deductibles and Premiums
Your medical deductible should be viewed not merely as a healthcare term, but as a key instrument in your financial strategy. Understanding its direct, inverse relationship with your insurance premium is what enables an intelligent, calculated decision—balancing immediate cash flow against potential future risks.
The relationship is straightforward: by agreeing to cover a larger portion of your initial medical costs (a higher deductible), you are rewarded by the insurer with a lower premium.
Essentially, a higher deductible communicates to the insurance company that you are willing to self-insure for smaller, more manageable events. This reduces their immediate risk and administrative burden, allowing them to offer a more favourable premium. A low deductible, conversely, places the insurer in a position of immediate liability, a higher risk that is reflected in a more substantial monthly premium.
This dynamic allows you to manage your health coverage as you would any other component of your financial portfolio, aligning it precisely with your personal risk tolerance and liquidity preferences.
Calculating Your Financial Breakeven Point
To make a truly informed decision, it is necessary to identify your financial 'breakeven point'. This is the threshold at which a high-deductible plan becomes more cost-effective than its low-deductible counterpart. This is not a theoretical exercise; it is a practical calculation that grounds your choice in quantitative analysis rather than intuition.
Here is a method for calculation:
Let us walk through a clear example to see this in action.
- Plan A (Low Deductible): $500 deductible, $5,400 annual premium.
- Plan B (High Deductible): $5,000 deductible, $2,700 annual premium.
Initially, your annual premium savings with Plan B are $2,700 ($5,400 – $2,700). The difference in your out-of-pocket exposure is $4,500 ($5,000 – $500).
If you remain healthy with minimal medical costs, you immediately realize that $2,700 saving. Even if you require significant care, the high-deductible plan remains the more economical option as long as your total medical bills for the year are below $3,200 (the $500 low deductible + your $2,700 in premium savings).
This breakeven analysis transforms a qualitative assessment into a strategic calculation. It allows you to quantify your risk and determine the exact level of healthcare expenditure at which the advantage of a lower premium is negated.
The Influence of Global Medical Inflation
This strategic balance is not static. It is subject to external economic forces, particularly global medical inflation. As the cost of healthcare services and new technologies escalates, insurers must adjust both premiums and deductibles to remain solvent. This is a critical factor, as it directly impacts the long-term value proposition of your chosen plan. You can learn more about why medical insurance premiums rise year after year in our detailed article.
Recently, global average medical inflation has been projected at 9.9% for 2024, continuing a trend of elevated rates. This is not uniform globally; regions such as Latin America and the Caribbean have projected increases of 13.6%, while Asia-Pacific is forecast at 9.2%. Insurers often respond to these pressures by raising deductibles to prevent premium increases from becoming untenable for their clients. You can find more insights on global medical trends in this WTW survey.
The chart below illustrates the fundamental payment sequence, clarifying who pays for what, and when.
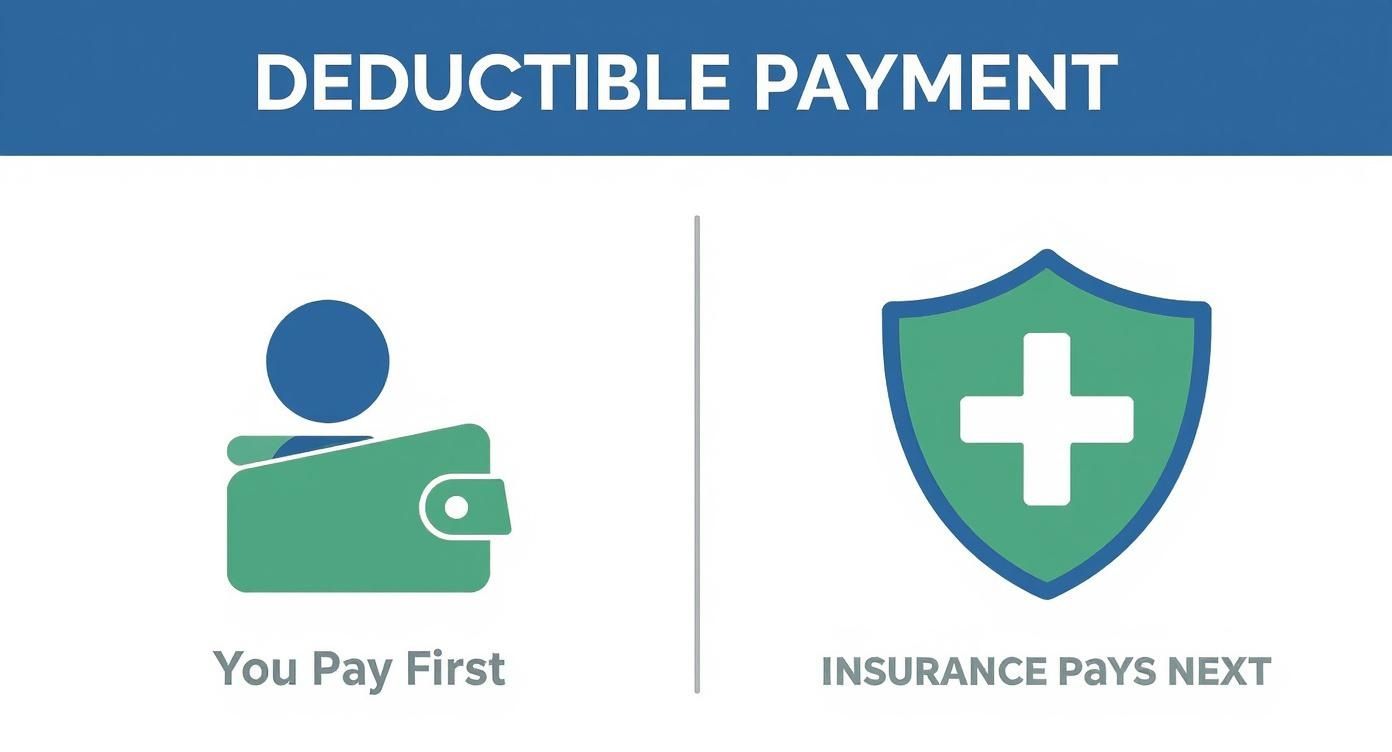
This visual reinforces the core principle: you cover initial costs up to your deductible limit. Only after you have met that amount does the financial responsibility shift to your insurer.
Navigating Deductibles in Global Medical Insurance
For any globally mobile professional, a dictionary definition of a medical deductible is insufficient. The critical skill is to translate this knowledge into a sophisticated strategy that aligns with the specific healthcare system of your country of residence. An International Private Medical Insurance (IPMI) plan offers exceptional flexibility, but its true value is only unlocked when your deductible is calibrated to the costs and regulations of your resident country.
Healthcare systems vary dramatically between financial hubs. A deductible strategy that yields substantial savings in one jurisdiction could be a costly miscalculation in another. Therefore, a rigorous analysis of how deductibles function in key expatriate cities is not a theoretical exercise—it is a critical step in building global health coverage that is both robust and cost-efficient.
A Comparative Look at Key Expat Hubs
Every major international city has a unique regulatory and market environment that influences your ideal deductible strategy. Local laws, the quality and cost of public versus private care, and the integration of state-sponsored programs all play a significant role. Let us examine three classic examples: Dubai, Singapore, and Switzerland.
-
Dubai: The Mandatory Coverage Model
Dubai mandates that all residents have health insurance, which has fostered a highly competitive market. For high-net-worth individuals, the government-mandated basic plans are seldom adequate, making a premier IPMI policy essential. Here, a deductible can be strategically employed to lower the premium on a comprehensive plan that provides access to leading private hospitals, while the basic mandatory plan may cover minor, routine check-ups. -
Singapore: The Integrated System
Singapore features a world-class healthcare system supported by Medisave, a national medical savings scheme. Expatriates on certain visas may be required to contribute. An astute IPMI strategy in Singapore often involves selecting a higher deductible to reduce premiums significantly. The IPMI plan would be reserved for major medical events, while Medisave or personal funds could be used for routine care that falls below the high deductible threshold. -
Switzerland: The Premium on Private Access
Switzerland has an excellent but notoriously expensive universal healthcare system. IPMI plans are frequently used to supplement this system, providing access to private rooms, choice of physicians, and reduced waiting times. A higher deductible on your IPMI policy makes this supplemental coverage far more affordable. It effectively becomes a tool to guarantee elite care for serious issues without paying a substantial premium for everyday health needs already covered by the mandatory basic insurance.
This comparative analysis reveals a core truth: a deductible is not chosen in isolation. It must be a calculated decision, informed by how your private plan interacts with the local healthcare environment.
A brief overview of how medical deductibles are typically utilized in the private insurance markets of major international cities can further clarify this point.
Deductible Strategies in Key Expat Hubs
| Expat Hub | Typical Deductible Range (IPMI) | Primary Use Case | Local Healthcare System Interaction |
|---|---|---|---|
| Hong Kong | $1,000 – $10,000 | Reduce premiums for comprehensive private cover; manage high costs of private specialists. | Supplements a strained public system to gain faster access to high-quality private care. |
| Singapore | $2,500 – $15,000 | Cost-sharing strategy; use MediShield Life/Integrated Shield Plans for smaller claims. | Often layered on top of mandatory local plans (ISPs) to cover deductibles or non-covered services. |
| United Kingdom | $500 – $5,000 | Bypass NHS waiting lists for elective procedures and gain access to private specialists. | Acts as a parallel system to the NHS, primarily for speed and choice rather than basic coverage. |
As is evident, the deductible is not merely a number; it is a strategic lever to align your coverage with local realities.
The Evolution of Deductibles and Rising Costs
The need for a sophisticated deductible strategy is becoming more urgent due to the relentless global trend of rising healthcare costs. Over the past few decades, deductibles have transformed from nominal amounts into substantial financial thresholds. For instance, in the early 2000s, the average individual deductible on an employer-sponsored health plan in the U.S. was under $500. By 2023, that figure had more than tripled to $1,735. This is not a minor adjustment; it is a fundamental shift in health plan architecture. You can delve deeper into how global trends are affecting plan costs by reading the full Aon report on medical rates.
This historical context makes one thing clear: a "set it and forget it" approach to selecting your deductible is no longer viable. As insurers raise these thresholds to manage their own risk in an inflationary environment, you must be equally proactive in structuring your coverage.
Aligning Your IPMI Deductible with Your Global Lifestyle
Ultimately, the primary advantage of an IPMI plan is its customisability. Your deductible is the main instrument for this, allowing you to fine-tune your coverage with precision. By understanding the local context, you can avoid overpaying for coverage you will not use or, more critically, finding yourself underinsured when a serious medical event occurs.
Your deductible choice should reflect a clear understanding of local healthcare access and costs. It is the mechanism that allows you to pay only for the level of risk you are not comfortable assuming yourself, ensuring your premium is allocated efficiently toward protecting against major financial shocks.
A well-chosen deductible transforms your IPMI policy from a generic safety net into a bespoke financial tool. It empowers you to navigate complex international healthcare systems with confidence, ensuring both your health and your wealth are diligently protected. To gain a better understanding of what these plans offer, you can discover more about the core benefits of international private medical insurance in our comprehensive guide.
Choosing Your Optimal Deductible: A Framework
Selecting the right medical deductible is not a simple cost-cutting exercise; it is a foundational component of your personal financial architecture. For a high-net-worth individual, the objective is not to find the cheapest option, but the most efficient one. It is about structuring your coverage so the insurance provides a fortress against major medical events, while you manage predictable, routine expenses yourself.
This transforms the very medical deductibles definition from a passive plan feature into an active tool for customisation. Achieving the correct balance demands a deliberate assessment of your health, finances, and the local healthcare landscape.
Assess Your Health and Risk Profile
The bedrock of any intelligent deductible strategy is a candid assessment of your likely healthcare needs. This is not an attempt to predict the future, but rather to make an informed forecast based on your personal and family health history. A clear-eyed view of your risk profile is what allows you to calibrate your deductible with precision.
Consider these factors:
- Chronic Conditions: Are you or a family member managing a long-term condition that necessitates regular physician visits, prescriptions, or monitoring?
- Family History: Are there hereditary conditions in your family that suggest a higher probability of future medical needs?
- Lifestyle and Age: Does your lifestyle involve activities with elevated risk, or are you at an age where healthcare utilization naturally tends to increase?
A clean bill of health and minimal prior medical usage might suggest a higher deductible, allowing you to retain the premium savings. Conversely, if you have predictable, ongoing medical costs, a lower deductible will almost certainly be more cost-effective over the long term.
Evaluate Your Financial Liquidity
Your deductible is, at its core, the amount you are willing to self-insure. This decision must be anchored in your financial reality—specifically, your cash flow and access to liquid funds. The right deductible is one you can meet without disrupting your broader financial plan.
Ask yourself two critical questions:
- What is your comfort level with self-funding? Determine the maximum out-of-pocket expense you could absorb for an unexpected medical event without experiencing financial strain.
- Can you cover the deductible instantly? You must ensure that the full deductible amount is available in cash or a highly liquid account, entirely separate from your long-term investments.
A well-chosen deductible should never compel you to liquidate assets or compromise your investment positions. It should align with your capacity to cover initial medical costs while your capital remains deployed in your primary financial strategy.
This analysis ensures your health plan acts as a shield for your wealth, not a drain on it. The premium savings from a higher deductible are only valuable if you possess the requisite liquidity to manage the risk you have assumed.
Align with Local Healthcare Costs
For an expatriate, a deductible cannot be chosen in a vacuum. It is imperative to benchmark it against the real-world cost of healthcare in your country of residence. What constitutes a "minor" medical expense varies dramatically between Singapore, London, and Hong Kong.
To structure your coverage effectively, you must understand the local terrain. Research the typical costs for common services that would fall under your deductible:
- Consultations: What is the prevailing rate for a visit to a General Practitioner or a specialist?
- Diagnostics: What is the actual cost of a standard set of blood tests or an MRI scan?
- Minor Procedures: What is the out-of-pocket price for a routine outpatient procedure?
By aligning your deductible with these local costs, you create a logical threshold. You can set it just above the level of your predictable annual expenses, ensuring you are not paying high premiums to cover costs you could easily manage yourself. This strategic move transforms your deductible into a powerful tool, ensuring your premium dollars are allocated where they matter most: protecting you from truly significant financial risk.
Frequently Asked Questions
Even with a clear strategy, certain specific questions invariably arise when fine-tuning an international health insurance plan. Clarifying these details is key to mastering your policy and protecting your health without jeopardizing your assets. Let us address the most common inquiries.
What Is the Difference Between a Deductible and an Out-of-Pocket Maximum?
This is a critical distinction.
Consider your deductible as the first financial hurdle. It is the fixed amount of money you pay from your own funds for covered medical care before your insurer begins to contribute.
The out-of-pocket maximum, in contrast, is your ultimate financial safety net. It represents the absolute ceiling on what you will spend in a policy year on your deductible, copayments, and coinsurance combined. Once you reach this figure, your insurer covers 100% of all eligible costs for the remainder of that year. This provides a safeguard against truly catastrophic medical expenses. Your deductible is one component of this larger protective limit.
Does a Deductible Apply to All Medical Services?
Not always, and this is where the quality of a premium IPMI plan becomes apparent. While your deductible will apply to most significant treatments, hospitalisations, and diagnostics, many high-end international plans waive it entirely for preventive services.
This often includes services such as:
- Annual physical examinations and health screenings.
- Routine immunisations and vaccinations.
- Preventive consultations designed to maintain wellness.
These services are frequently covered from day one, with no requirement to meet your deductible first. This is a sophisticated structure that encourages proactive health management, reserving the deductible for unexpected, more serious medical events.
How Do Family Deductibles Work?
When insuring a family, you will encounter two primary types of deductibles, and the difference can have a significant impact on your budget.
An individual deductible means each person on the policy has a separate deductible to meet. If your plan has a $2,000 individual deductible, each family member must satisfy that $2,000 threshold with their own expenses before the insurance begins to pay for their care.
An aggregate family deductible, however, pools all members' expenses together. For example, if the family deductible is $6,000, it is irrelevant which family member incurs the costs. Once the combined medical bills from everyone on the plan reach that $6,000 mark—whether from one person's major surgery or several smaller issues across the family—the insurer starts covering costs for everyone for the rest of the year.
Navigating these details is precisely where expert guidance becomes invaluable. At Riviera Expat, we specialize in structuring sophisticated IPMI plans that align with your unique financial and lifestyle requirements. We provide the clarity and control you need to make confident healthcare decisions. Schedule your complimentary consultation with Riviera Expat today.

